Each year about 795,000 people experience a new or recurrent stroke, which is the nation’s third leading cause of death. On average, someone suffers a stroke every 40 seconds and someone dies of a stroke every 3.1 minutes. Stroke is a leading cause of serious, long-term disability in the United States, with about 4.7 million stroke survivors alive today.
With seven neurologists and nine neurosurgeons on staff, the Stroke Center at Ochsner Lafayette General Medical Center offers comprehensive stroke care and recovery for patients. Backed by a host of critical care providers and neuroscience specialists, stroke patients get coordinated care from a variety of departments to effectively address their condition.
What Is a Stroke?
A stroke occurs when the blood supply to an artery in the brain is blocked (a clot), or a blood vessel breaks, causing brain cells in the area to die. Brain cells do not regenerate. The problems experienced after a stroke, like the inability to move one side of the body, numbness on one side of the body, speech or visual problems, are usually a result of brain damage.
People who have had one stroke are at risk of having another stroke. It is important that you practice stroke prevention now, and this guide will help you and your family do just that.
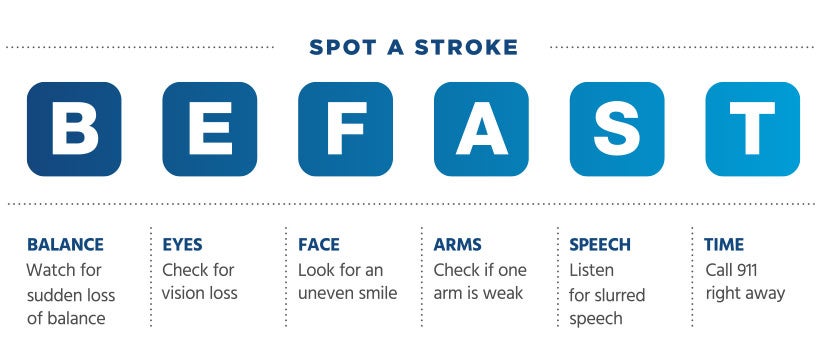
Warning signs and symptoms of stroke:
- Sudden numbness or weakness of the face, arm or leg, especially on one side of the body
- Sudden confusion, trouble speaking or understanding
- Sudden trouble seeing in one or both eyes
- Sudden trouble walking, dizziness, loss of balance or coordination
- Sudden, severe headache with no known cause
What to do if someone is having symptoms of a stroke:
- Not all the warning signs occur in every stroke. Don’t ignore signs of stroke, even if they go away!
- Check the time. When did the first warning sign or symptom start? You or the person who is with you will be asked this important question later. This is very important because, if given within four and a half hours of the start of symptoms, a clot-busting drug can reduce long-term disability for the most common type of stroke.
- If you have one or more stroke symptom(s) that last more than a few minutes, don’t delay! Immediately call 9-1-1 or the emergency medical service (EMS) number so an ambulance (ideally with advanced life support) can quickly be sent for you. Do not drive yourself. When communicating with EMS or the hospital, make sure and use the word “STROKE”.
- If you are with someone who may be having stroke symptoms, immediately call 9-1-1 or the EMS. Expect the person to resist going to the hospital. Don’t take “no” for an answer because “Time Lost is Brain Lost.”
Stroke Prevention
Stroke affects everyone differently; with varying outcomes from mild to devastating. Below are helpful information sheets from the * * National Stroke Association on the different aspects of stroke recovery, care and rehabilitation.
- To prevent a stroke from recurring, it is imperative to follow your doctor’s recommendations.
- You need to continue the medications prescribed after you leave the hospital in order to reduce your risk of another stroke or other cardiovascular event. Medications must be taken as prescribed by your doctor in order for them to be effective in reducing your risk of another stroke.
- The medicines are most effective when they help you reach the goal of lowering each of your risk factors. Therefore, the doses of these medicines will likely need to be adjusted in order for them to be effective, based on blood tests and other measurements made by your doctor after you leave the hospital. Don’t stop your medications without speaking to your physician first.
- It is important that you receive regular medical care after you leave the hospital, since this is how the doctors can measure the effectiveness of the treatments and make sure your medicine are adjusted properly.
- Make sure you have a plan for which doctor(s) you will see and when to see them after you leave the hospital and be sure to have your list of medications with you for all doctor visits.
Quality Outcomes
The two main treatment options for stroke are tPA (clot busting medication) and thrombectomy (reopening of the blocked blood vessel).
When patients arrive with new stroke symptoms, it is our goal to administer treatment as soon as possible. In 2021, Ochsner Lafayette General Medical Center’s median “Door-to-Needle” time was 38.5 minutes.
Of the patients who received thrombectomy, 94% were recanalized (reopening of the blocked blood vessel). Among those patients, 84% had a TICI score of 2B or 3. A TICI score is a way of grading the level of success during recanalization therapy on a range from 0—3. A score of 2B or 3 is considered a successful recanalization.
In addition to recanalization, we also help improve quality of life outcomes post-stroke through patient rehabilitation services. Therapy and progress tracking is provided through Ochsner Lafayette General Orthopedic Hospital, which is part of the Ochsner Lafayette General Medical Center campus. Patients can seamlessly transfer from critical stroke care and recovery to rehabilitation, where they are aided by a team of specialists to improve coordination and motor skills needed for daily living.
LEARN ABOUT OUR NEUROLOGY SERVICES
Stroke Recovery Resources
After a stroke, it may seem that no one understands what you’re going through. The Acadiana Stroke Support Group is here to help by providing a support system for survivors and families, a life raft of hope and understanding on the way to recovery. This is a community service provided by Ochsner Lafayette General. Anyone, regardless of where you seek medical treatment, can attend the meetings. Click Here to see the complete list of meetings.